Printable Tb Test Template
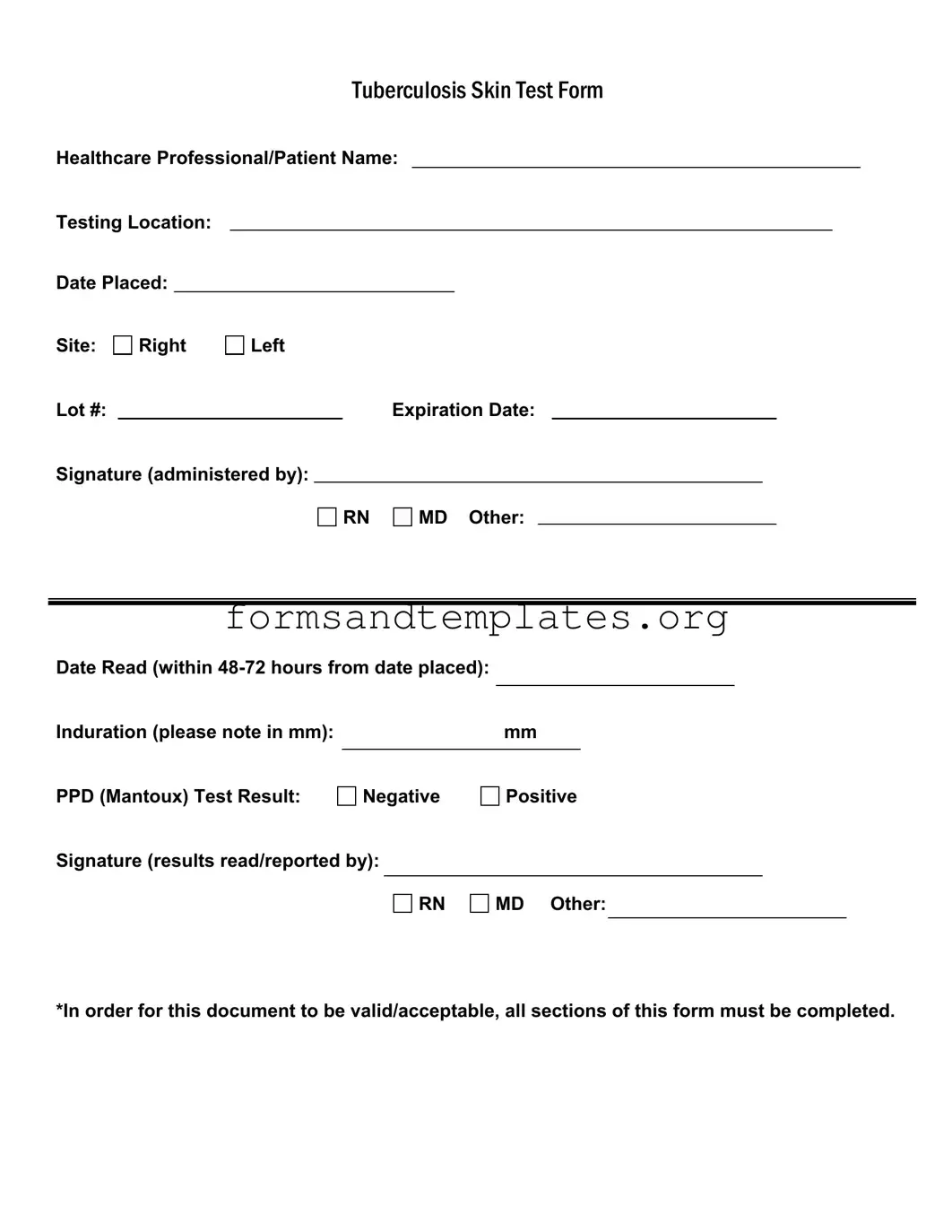
The Tuberculosis (TB) Skin Test form is a crucial document used in the assessment and monitoring of tuberculosis exposure and infection. This form captures essential information about both the healthcare professional administering the test and the patient receiving it. Key details include the names of the healthcare professional and patient, the testing location, and the date the test was placed. Additionally, the form specifies the site of administration, whether on the right or left arm, along with the lot number and expiration date of the testing material. A signature from the administering professional, which may be a registered nurse (RN), medical doctor (MD), or other qualified personnel, is required to validate the test. The form also mandates that the results be read within 48 to 72 hours of placement, recording the induration measurement in millimeters. The outcome of the PPD (Mantoux) test is clearly indicated as either negative or positive. Finally, a signature from the professional who reads and reports the results is necessary, ensuring that all sections of the form are completed for it to be valid and acceptable.
Common mistakes
-
Incomplete Information: One common mistake is not filling out all required sections of the form. Every field, including the healthcare professional's name, testing location, and signature, must be completed for the document to be valid.
-
Incorrect Dates: Failing to accurately record the date the test was placed or the date it was read can lead to complications. The test must be read within 48-72 hours, and missing this timeframe can invalidate the results.
-
Improper Induration Measurement: When measuring the induration, it's essential to note the measurement in millimeters correctly. An inaccurate reading can lead to misinterpretation of the test results, affecting patient care.
-
Signature Errors: Not providing the appropriate signature for both the administration and the reading of the test can render the form incomplete. Ensure that the signature reflects the correct title, whether it be RN, MD, or another designation.
Find Common Documents
Dd Form 2870 - By submitting the DD 2870, you help ensure your dental records are up to date.
For those looking to navigate potential liabilities, understanding the importance of a Hold Harmless Agreement form is crucial in many professional and social situations. This form, which can help mitigate risks associated with specific activities, is essential for ensuring that all parties are aware of their responsibilities. You can learn more by visiting the website that offers valuable insights on the topic, including a well-crafted Hold Harmless Agreement template designed for various needs: understanding the Hold Harmless Agreement form.
Pre Trip Inspection Class a Pdf With Pictures - Helps drivers verify their vehicle is road-ready.
Key takeaways
When filling out and using the TB Test form, it is essential to follow specific guidelines to ensure accuracy and compliance. Here are key takeaways to consider:
- Complete All Sections: Every part of the form must be filled out for it to be valid. Incomplete forms may lead to delays or rejection.
- Identify the Testing Location: Clearly state where the test is being conducted. This information is crucial for tracking and record-keeping.
- Record Dates Accurately: Note both the date the test is placed and the date it is read. The reading must occur within 48-72 hours of placement.
- Induration Measurement: Measure and record the induration in millimeters. This measurement is critical for determining the test result.
- Test Results: Clearly indicate whether the PPD (Mantoux) test result is negative or positive. This will guide further medical decisions.
- Signature Requirement: Ensure that the form is signed by the healthcare professional administering the test and the one reading the results.
- Expiration Date: Check the expiration date of the lot number used for the test. Using expired materials can compromise results.
- Documentation: Keep a copy of the completed form for your records. This can be important for future medical evaluations or requirements.
Tb Test Example
|
|
|
|
|
TUBERCULOSISSKINTESTFORM |
||||||||
Healthcare Professional/Patient Name: |
|||||||||||||
Testing Location: |
|
|
|
|
|
|
|
|
|
|
|
||
Date Placed: |
|
|
|
|
|
|
|
|
|
|
|
|
|
Site: |
Right |
Left |
|
|
|
|
|
|
|
|
|||
Lot #: |
|
|
|
|
|
Expiration Date: |
|
|
|||||
Signature (administered by): |
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
RN |
|
MD Other: |
|
|
|
|||
Date Read (within |
|
|
|
|
|
|
|
Induration (please note in mm): |
|
mm |
|
PPD (Mantoux) Test Result: |
|
|
|
Negative |
Positive |
||
Signature (results read/reported by):
RN
MD Other:
*In order for this document to be valid/acceptable, all sections of this form must be completed.
Understanding Tb Test
What is the purpose of the TB Test form?
The TB Test form is used to document the administration and results of the Tuberculosis skin test, also known as the PPD or Mantoux test. This form ensures that all necessary information is recorded for proper evaluation of the test results.
Who should fill out the TB Test form?
The form should be completed by a healthcare professional administering the test. This includes registered nurses (RNs), medical doctors (MDs), or other qualified personnel. The patient’s information must also be included on the form.
What information is required on the TB Test form?
The TB Test form requires the following information:
- Healthcare Professional/Patient Name
- Testing Location
- Date Placed
- Site of injection (Right or Left)
- Lot number and expiration date of the PPD
- Signature of the administering professional
- Date Read (within 48-72 hours from date placed)
- Induration measurement in mm
- PPD Test Result (Negative or Positive)
- Signature of the professional reading/reporting the results
What does the induration measurement indicate?
The induration measurement, noted in millimeters (mm), indicates the size of the raised area at the injection site. This measurement is critical for determining whether the test result is positive or negative. A larger induration may suggest exposure to TB.
How soon should the results be read?
Results must be read within 48 to 72 hours after the test is administered. Reading the results outside this timeframe may lead to inaccurate interpretations.
What does a positive result mean?
A positive result indicates that the individual has been exposed to the TB bacteria. It does not necessarily mean that the person has active tuberculosis. Further evaluation, such as a chest X-ray or additional tests, may be required to determine if the infection is active.
What does a negative result mean?
A negative result suggests that there is no evidence of TB infection. However, it is important to note that false negatives can occur, especially in individuals with weakened immune systems or recent exposures.
What should I do if the form is incomplete?
If any section of the TB Test form is incomplete, the document may be considered invalid. Ensure that all required fields are filled out accurately before submission. This includes signatures, dates, and measurements.
Where can I obtain a TB Test form?
TB Test forms can typically be obtained from healthcare facilities, clinics, or public health departments. Many organizations also provide downloadable versions online for convenience.
How to Use Tb Test
Completing the Tb Test form is essential for ensuring accurate results and proper documentation. Follow these steps carefully to fill out the form correctly.
- Write the name of the healthcare professional and patient at the top of the form.
- Fill in the testing location where the test is being conducted.
- Enter the date the test was placed.
- Indicate the site of the test by marking either Right or Left.
- Record the lot number of the test.
- Fill in the expiration date of the test.
- Have the healthcare professional sign in the section labeled "Signature (administered by)." Choose RN, MD, or Other as applicable.
- After 48-72 hours, record the date the results were read.
- Measure the induration in millimeters and write this number in the designated space.
- Mark the PPD (Mantoux) Test Result as Negative or Positive.
- Have the healthcare professional sign again in the section labeled "Signature (results read/reported by)." Choose RN, MD, or Other as applicable.
Make sure all sections are filled out completely. This ensures that the document is valid and acceptable for further processing.