Printable Annual Physical Examination Template
The Annual Physical Examination form serves as a crucial tool for both patients and healthcare providers, ensuring a comprehensive assessment of an individual's health status. This form is designed to collect essential information prior to a medical appointment, including personal details such as name, date of birth, and contact information. It prompts patients to disclose significant health conditions and a summary of their medical history, which can help in diagnosing potential issues. Additionally, the form requires a detailed list of current medications, allergies, and immunization records, ensuring that healthcare providers have a complete picture of the patient's medical background. Sections on tuberculosis screening and other diagnostic tests further enhance the thoroughness of the evaluation. The second part of the form focuses on the general physical examination, capturing vital signs and evaluations of various body systems. This structured approach not only facilitates a more efficient examination process but also promotes proactive health management by documenting recommendations for future care, lifestyle adjustments, and any necessary follow-ups. By accurately completing this form, individuals can significantly contribute to their own health outcomes while minimizing the need for return visits.
Common mistakes
-
Incomplete Personal Information: Many individuals fail to fill out all required fields, such as the date of birth or Social Security Number. This can lead to delays in processing the form and may require additional visits.
-
Neglecting to List Current Medications: Some people forget to include all medications they are currently taking. Omitting this information can hinder the physician's ability to provide appropriate care.
-
Ignoring Allergies: A common mistake is not listing allergies or sensitivities. This oversight can result in serious health risks if the physician prescribes medication that the patient is allergic to.
-
Inaccurate Health History: Individuals often provide vague or incomplete medical histories. This lack of detail can prevent healthcare providers from understanding the patient's full health context.
-
Overlooking Follow-Up Recommendations: After the examination, patients sometimes neglect to document or follow through on recommended tests or consultations. This can lead to missed opportunities for necessary care.
Find Common Documents
Accord Forms - This form can be critical during insurance renewals or policy changes.
The California Motor Vehicle Bill of Sale form is not only crucial for legally documenting the sale of a vehicle but also ensures that both parties have a clear understanding of the terms involved. By providing essential information such as the vehicle's identification number and sale price, the form minimizes the risk of disputes. For those looking to easily complete this necessary paperwork, helpful resources can be found at California Templates.
Terminating Parental Rights in Sc - This form is essential for parents considering the termination of their legal responsibilities towards their child.
What Is an Abn in Healthcare - Patients must sign this notice to acknowledge their awareness of potential costs.
Key takeaways
Completing the Annual Physical Examination form accurately is essential for ensuring a smooth medical appointment and comprehensive health evaluation. Here are key takeaways to consider:
- Complete All Sections: Fill out every section of the form to avoid delays and return visits. This includes personal information, medical history, and current medications.
- Medication Details: List all current medications, including the name, dosage, frequency, and prescribing physician. Attach additional pages if necessary.
- Allergies and Sensitivities: Clearly indicate any allergies or sensitivities to medications or other substances to inform the healthcare provider.
- Immunization Records: Provide accurate dates for immunizations, including Tetanus, Hepatitis B, and Influenza. This helps in assessing vaccination status.
- Health Screening Tests: Document any relevant health screenings, such as mammograms or prostate exams, along with their results. This information is crucial for ongoing health management.
- Communicable Diseases: Indicate whether the individual is free from communicable diseases. If not, specify precautions to prevent transmission.
- Changes in Health Status: Note any changes in health since the last examination. This information can influence the current evaluation and treatment plan.
- Follow-Up Recommendations: Pay attention to any recommendations for further evaluations, treatments, or lifestyle changes provided by the physician after the examination.
Annual Physical Examination Example
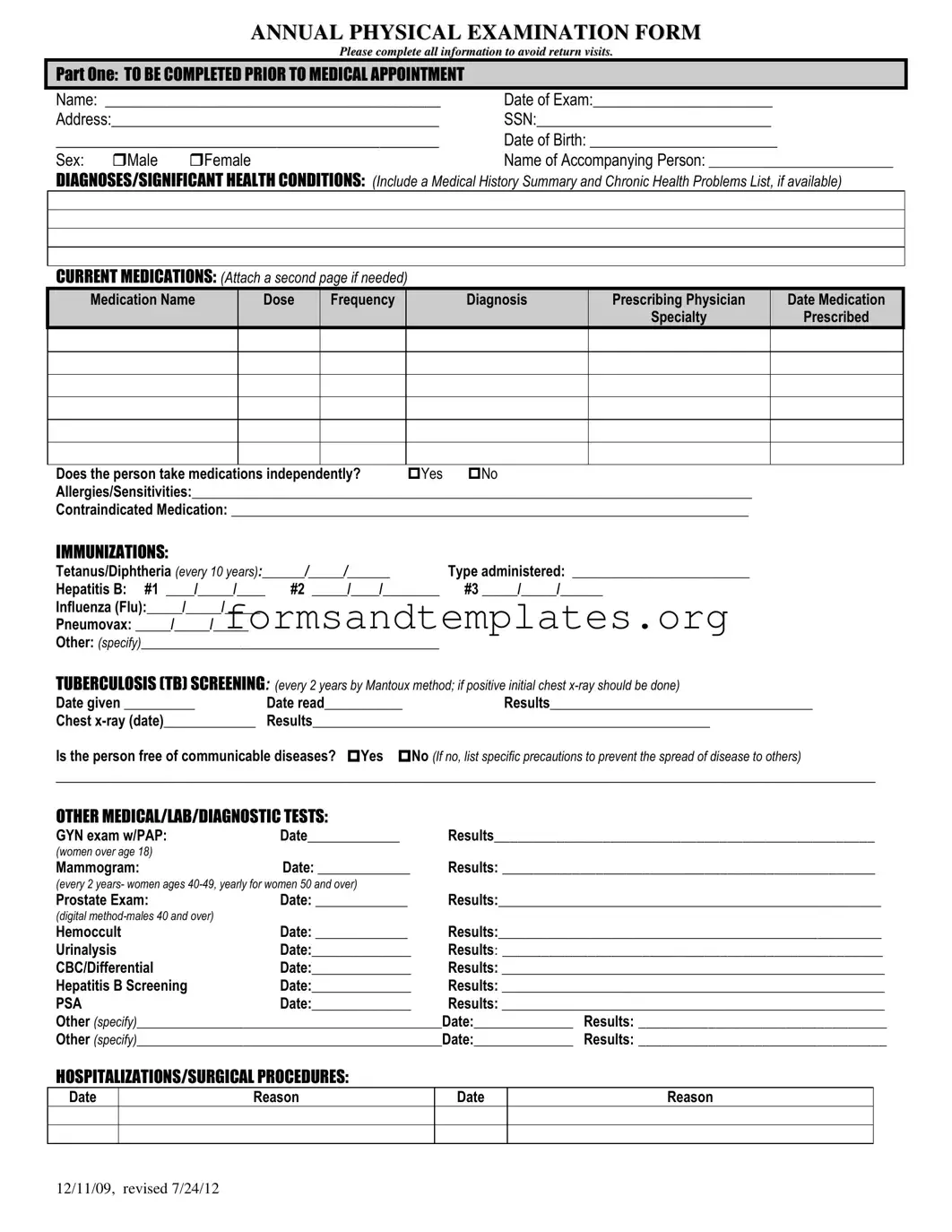
ANNUAL PHYSICAL EXAMINATION FORM
Please complete all information to avoid return visits.
PART ONE: TO BE COMPLETED PRIOR TO MEDICAL APPOINTMENT
Name: ___________________________________________ |
Date of Exam:_______________________ |
Address:__________________________________________ |
SSN:______________________________ |
_____________________________________________ |
Date of Birth: ________________________ |
||
Sex: |
Male |
Female |
Name of Accompanying Person: __________________________ |
DIAGNOSES/SIGNIFICANT HEALTH CONDITIONS: (Include a Medical History Summary and Chronic Health Problems List, if available)
CURRENT MEDICATIONS: (Attach a second page if needed)
Medication Name |
Dose |
Frequency |
Diagnosis |
Prescribing Physician |
Date Medication |
|
|
|
|
Specialty |
Prescribed |
Does the person take medications independently? |
Yes |
No |
Allergies/Sensitivities:_______________________________________________________________________________ |
||
Contraindicated Medication: _________________________________________________________________________
IMMUNIZATIONS:
Tetanus/Diphtheria (every 10 years):______/_____/______ |
Type administered: _________________________ |
|
Hepatitis B: #1 ____/_____/____ |
#2 _____/____/________ |
#3 _____/_____/______ |
Influenza (Flu):_____/_____/_____ |
|
|
Pneumovax: _____/_____/_____ |
|
|
Other: (specify)__________________________________________ |
|
|
TUBERCULOSIS (TB) SCREENING: (every 2 years by Mantoux method; if positive initial chest |
||
Date given __________ |
Date read___________ |
Results_____________________________________ |
Chest |
Results________________________________________________________ |
|
Is the person free of communicable diseases? Yes No (If no, list specific precautions to prevent the spread of disease to others)
_________________________________________________________________________________________________________
OTHER MEDICAL/LAB/DIAGNOSTIC TESTS:
GYN exam w/PAP: |
Date_____________ |
Results_________________________________________________ |
(women over age 18) |
|
|
Mammogram: |
Date: _____________ |
Results: ________________________________________________ |
(every 2 years- women ages
Prostate Exam: |
Date: _____________ |
Results:______________________________________________________ |
|
(digital |
|
|
|
Hemoccult |
Date: _____________ |
Results:______________________________________________________ |
|
Urinalysis |
Date:______________ |
Results: _________________________________________________ |
|
CBC/Differential |
Date:______________ |
Results: ______________________________________________________ |
|
Hepatitis B Screening |
Date:______________ |
Results: ______________________________________________________ |
|
PSA |
Date:______________ |
Results: ______________________________________________________ |
|
Other (specify)___________________________________________Date:______________ |
Results: ________________________________ |
||
Other (specify)___________________________________________Date:______________ |
Results: ________________________________ |
||
HOSPITALIZATIONS/SURGICAL PROCEDURES:
Date
Reason
Date
Reason
12/11/09, revised 7/24/12

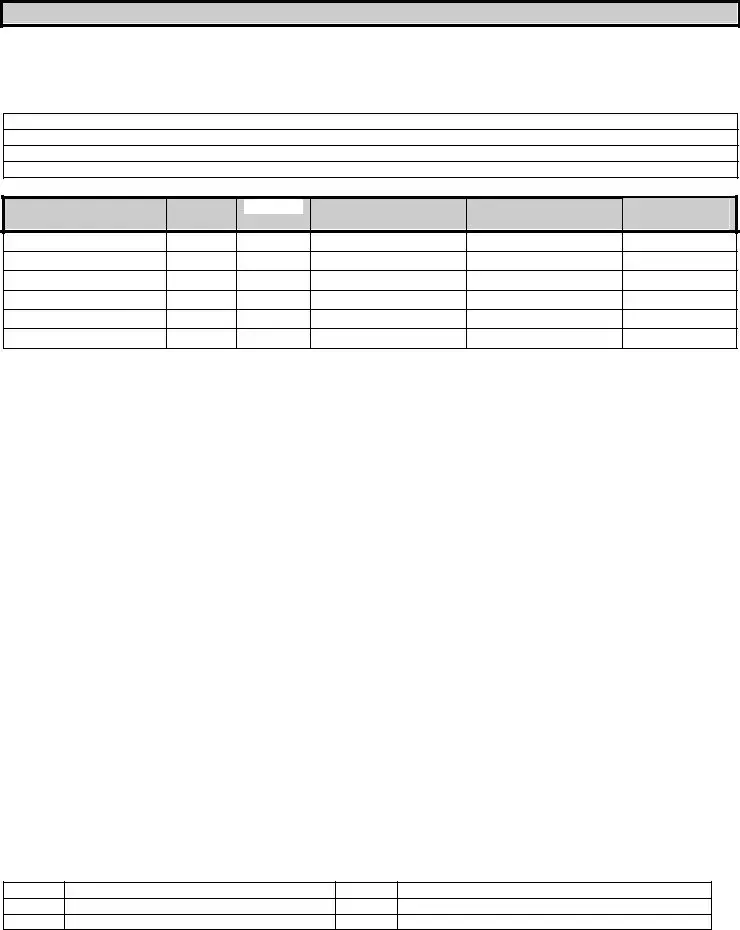
PART TWO: GENERAL PHYSICAL EXAMINATION
|
|
|
|
|
Please complete all information to avoid return visits. |
|
|
|
|
|
Blood Pressure:______ /_______ Pulse:_________ |
Respirations:_________ Temp:_________ Height:_________ |
Weight:_________ |
||||
|
|
EVALUATION OF SYSTEMS |
|
|
|
|
||
|
|
|
|
|
|
|
||
|
|
System Name |
|
Normal Findings? |
Comments/Description |
|
||
|
|
Eyes |
|
Yes |
No |
|
|
|
|
|
Ears |
|
Yes |
No |
|
|
|
|
|
Nose |
|
Yes |
No |
|
|
|
|
|
Mouth/Throat |
|
Yes |
No |
|
|
|
|
|
Head/Face/Neck |
|
Yes |
No |
|
|
|
|
|
Breasts |
|
Yes |
No |
|
|
|
|
|
Lungs |
|
Yes |
No |
|
|
|
|
|
Cardiovascular |
|
Yes |
No |
|
|
|
|
|
Extremities |
|
Yes |
No |
|
|
|
|
|
Abdomen |
|
Yes |
No |
|
|
|
|
|
Gastrointestinal |
|
Yes |
No |
|
|
|
|
|
Musculoskeletal |
|
Yes |
No |
|
|
|
|
|
Integumentary |
|
Yes |
No |
|
|
|
|
|
Renal/Urinary |
|
Yes |
No |
|
|
|
|
|
Reproductive |
|
Yes |
No |
|
|
|
|
|
Lymphatic |
|
Yes |
No |
|
|
|
|
|
Endocrine |
|
Yes |
No |
|
|
|
|
|
Nervous System |
|
Yes |
No |
|
|
|
|
|
VISION SCREENING |
|
Yes |
No |
Is further evaluation recommended by specialist? |
Yes |
No |
|
|
HEARING SCREENING |
|
Yes |
No |
Is further evaluation recommended by specialist? |
Yes |
No |
|
|
ADDITIONAL COMMENTS: |
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
Medical history summary reviewed? |
Yes |
No |
|
|
||
Medication added, changed, or deleted: (from this appointment)__________________________________________________________
Special medication considerations or side effects: ________________________________________________________________
Recommendations for health maintenance: (include need for lab work at regular intervals, treatments, therapies, exercise, hygiene, weight control, etc.)
___________________________________________________________________________________________________________
Recommendations for manual breast exam or manual testicular exam: (include who will perform and frequency)____________________
___________________________________________________________________________________________________________
Recommended diet and special instructions: ____________________________________________________________________
Information pertinent to diagnosis and treatment in case of emergency:
___________________________________________________________________________________________________________
Limitations or restrictions for activities (including work day, lifting, standing, and bending): No Yes (specify)
___________________________________________________________________________________________________________ |
|||
Does this person use adaptive equipment? |
No |
Yes (specify):________________________________________________ |
|
Change in health status from previous year? No |
Yes (specify):_________________________________________________ |
||
This individual is recommended for ICF/ID level of care? (see attached explanation) Yes |
No |
||
Specialty consults recommended? No |
Yes (specify):_________________________________________________________ |
||
Seizure Disorder present? No Yes (specify type):__________________________________ Date of Last Seizure: ______________ |
|||
________________________________ |
_______________________________ |
_________________ |
|
Name of Physician (please print) |
Physician’s Signature |
|
Date |
Physician Address: _____________________________________________ |
Physician Phone Number: ____________________________ |
||
12/11/09, revised 7/24/12
Understanding Annual Physical Examination
What is the purpose of the Annual Physical Examination form?
The Annual Physical Examination form is designed to collect essential health information from patients before their medical appointments. Completing this form helps healthcare providers assess an individual's health status accurately. It includes sections for personal information, medical history, current medications, allergies, immunizations, and results from various medical tests. By providing comprehensive details, patients can help ensure a thorough evaluation during their visit, which may lead to better health outcomes.
How should I fill out the medication section of the form?
When filling out the medication section, list all current medications, including prescription drugs, over-the-counter medications, and supplements. For each medication, include the following details:
- Medication Name
- Dose
- Frequency of use
- Diagnosis for which it was prescribed
- Prescribing physician's name
- Date medication was prescribed
- Specialty of the prescribing physician
If you take multiple medications, feel free to attach an additional page. It is also important to indicate whether you take these medications independently or require assistance. This information is crucial for your healthcare provider to manage your treatment effectively.
What should I do if I have allergies or sensitivities?
If you have allergies or sensitivities, it is essential to disclose this information on the form. Clearly list any known allergies, including food, medication, or environmental factors. Additionally, specify any contraindicated medications that you should avoid. This information helps healthcare providers prevent adverse reactions during treatment and ensures your safety during the examination and any subsequent procedures.
What happens if I do not complete the form accurately?
Inaccurate or incomplete information on the Annual Physical Examination form may lead to delays in your medical care. If critical sections are left blank or filled out incorrectly, you may need to return for additional visits to provide the necessary information. To avoid this, take your time when completing the form and review it for accuracy before submission. If you have questions or need assistance, consider reaching out to your healthcare provider for guidance.
How to Use Annual Physical Examination
Completing the Annual Physical Examination form is an essential step to ensure that your upcoming medical appointment goes smoothly. By providing accurate and comprehensive information, you help your healthcare provider understand your health needs better. Follow these steps to fill out the form correctly.
- Begin with Part One. Write your full name in the designated space.
- Fill in the Date of Exam.
- Provide your complete address.
- Enter your Social Security Number (SSN).
- Input your Date of Birth and select your sex by checking the appropriate box.
- List the name of any accompanying person.
- Detail any diagnoses or significant health conditions, including a medical history summary if available.
- Document your current medications. Include the name, dose, frequency, diagnosis, prescribing physician, and date prescribed. If necessary, attach an additional page.
- Indicate whether you take medications independently by checking "Yes" or "No."
- List any allergies or sensitivities you have.
- Note any contraindicated medications.
- Fill in your immunization history, including dates and types of vaccinations.
- Complete the tuberculosis screening section, noting the date given and date read, along with results.
- Provide information about any other medical, lab, or diagnostic tests you have undergone, including dates and results.
- Document any hospitalizations or surgical procedures by listing the date and reason.
- Move to Part Two and record your vital signs: blood pressure, pulse, respirations, temperature, height, and weight.
- Evaluate each system listed. Indicate whether findings are normal by checking "Yes" or "No" and provide comments if necessary.
- Complete the vision and hearing screening sections, noting if further evaluation is recommended.
- Provide any additional comments regarding your medical history, medications, recommendations for health maintenance, and any special instructions.
- Indicate any limitations or restrictions for activities, checking "Yes" or "No" and specifying if applicable.
- Note whether you use adaptive equipment and if there has been a change in health status from the previous year.
- Finally, have your physician print their name, sign the form, and provide their address and phone number.
Once you have completed the form, review it for accuracy. Make sure all sections are filled out to avoid any delays during your appointment. Bring the form with you to your medical visit.